From ‘Possession’ to ‘No Cure’: Experts Address 5 Schizophrenia Myths Too Many Indians Still Believe
What would you do if your mind started playing tricks on you – if familiar voices suddenly sounded strange or shadows on the wall began whispering your name? What if the people around you stopped seeing you and only saw a diagnosis?
For thousands of people in India, this isn’t fiction. It’s schizophrenia – a condition often shrouded in silence, feared more than it’s understood.
Even as mental health becomes a growing conversation in India, schizophrenia remains stuck in the shadows. It’s reduced to a plot twist in a thriller, a punchline in casual conversation, or a label no one wants to claim. The word alone can change how someone is seen, from a neighbour or colleague to someone “not quite right.”
 Schizophrenia is still a hushed up topic in today’s India. Picture source: Shutterstock
Schizophrenia is still a hushed up topic in today’s India. Picture source: Shutterstock
But how much of what we think we know is actually true?
To separate fact from fear, The Better India spoke to Dr. Mala Khanna, a clinical psychologist who has spent years working with people diagnosed with schizophrenia. From busting myths like “split personality” to sharing real stories of resilience, Dr. Khanna invites us to see beyond the stigma and into the very human experience behind the diagnosis. Joining her is clinical psychologist Dr. Shweta Sharma, who adds crucial context about symptoms, trauma, and the road to recovery.
Myth 1: “Schizophrenia means having a split personality”
This is one of the most common and misleading myths about schizophrenia.
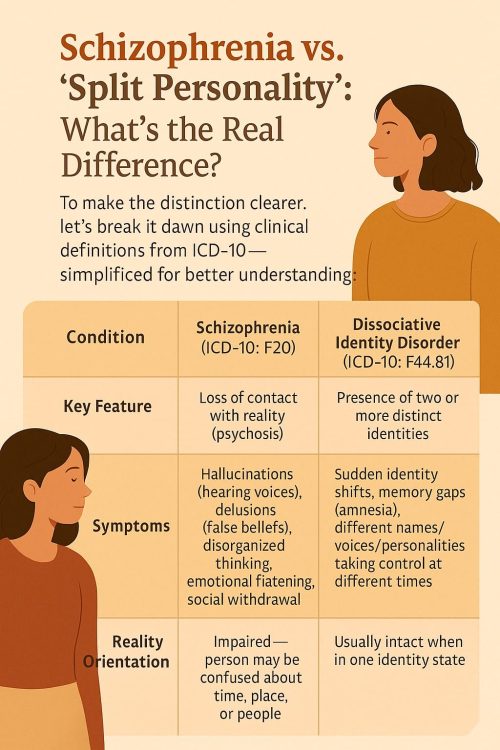
“People often confuse schizophrenia with Dissociative Identity Disorder (DID), where someone has different identity states. But schizophrenia has nothing to do with ‘split personalities’,” Dr. Khanna points out.
Dr. Shweta Sharma elaborates, “One of the most common and misleading myths in India is that schizophrenia means ‘split personality.’ This confusion leads to stigma, fear, and delayed treatment. But let’s set the record straight. Schizophrenia is a chronic, severe mental health condition that affects a person’s thoughts, emotions, and behaviours. It involves psychotic symptoms like hallucinations, delusions, disorganised thinking, social withdrawal, and flattened affect.”
“In schizophrenia, the core disturbance is in reality orientation, the person often loses touch with reality. This impaired reality testing is a key feature, and it can affect:
- Time orientation (confused about day/time)
- Place orientation (unsure where they are),
- Person orientation (mistrust or misidentification of others),
- Situation orientation (misinterpreting context, such as thinking they are in danger when they are not),” she adds.
In contrast, Dissociative Identity Disorder (DID), which people mistakenly refer to as “split personality”, involves two or more distinct identities or personality states that alternate in controlling the individual’s behavior. “So, schizophrenia is not about ‘having two minds.’ It’s about a disruption in perceiving and processing reality. That distinction is crucial for both clinical understanding and reducing stigma,” she says.
 One might confuse schizophrenia with having a split personality.
One might confuse schizophrenia with having a split personality.
Think of it this way: a person with schizophrenia may hear voices that aren’t there or believe things that others don’t, like feeling watched when they’re not. It affects how someone understands and responds to reality. But they don’t “switch personalities” or become someone else entirely, as often shown in films or TV.
The confusion isn’t just a harmless mix-up — it changes how we see people. “When people think ‘split personality,’ they assume instability or danger, and that makes stigma worse,” Dr. Khanna adds.
And that stigma can be damaging. It can isolate people, prevent them from seeking help, and deepen the fear around something that’s already misunderstood. Understanding the difference is the first step to treating people with empathy, not fear.
Myth 2: “People with schizophrenia are always dangerous”
Movies often show people with schizophrenia as violent or unpredictable — someone lashing out, losing control, or whispering to themselves before doing something terrifying. But real life is very different. In reality, schizophrenia often looks quieter, more inward, and far more complex.
Imagine someone who spends their afternoons sketching, listening to music, and helping around the house. They’re gentle, kind, and perhaps a little withdrawn. On some days, they might seem distant or distracted — maybe they’re hearing a voice no one else can hear or feel convinced that people are watching them, whispering things that aren’t really being said.
What you’re seeing isn’t danger. You’re seeing someone trying to make sense of a world that suddenly feels unfamiliar or overwhelming.
“Hallucinations are when someone hears, sees, or feels something that isn’t really there. Delusions are fixed false beliefs, like thinking people are trying to harm you, or that you have extraordinary powers,” Dr. Khanna explained. “These symptoms are different for each person and don’t make someone dangerous.”
In fact, individuals with schizophrenia are more likely to be vulnerable to harm than to cause it. Many live with fear, confusion, or distress, not aggression. The assumption that someone with schizophrenia is unsafe often leads to isolation and shame, making recovery even harder.
Myth 3: “They can’t live normal lives”
A diagnosis of schizophrenia doesn’t mean life stops. With access to the right care, many people continue to work, build relationships, raise families, and live independently.
“It’s entirely possible,” says Dr. Khanna. “But the key is consistent treatment, which includes regular medication, therapy, and strong support from family or caregivers.” She emphasises that schizophrenia requires ongoing care, and stopping treatment abruptly can lead to relapses. But stability and fulfilment are very much within reach.
“We’ve seen people return to jobs, reconnect with loved ones, and manage their symptoms effectively. It’s not hopeless.”
 Early trauma, emotional neglect, and abuse can all contribute to schizophrenia. Picture source: Shutterstock
Early trauma, emotional neglect, and abuse can all contribute to schizophrenia. Picture source: Shutterstock
Dr. Sharma adds, “Schizophrenia is not like a physical illness where we can always talk in terms of a full cure. Instead, it is managed through a long-term recovery model.”
“Recovery means reduction of symptoms, improved functioning, and a return to meaningful life roles. Many individuals live independently, maintain jobs, and have fulfilling relationships. The earlier the intervention, the better the outcome.”
Myth 4: “Medicines alone can fix it”
While medication plays a crucial role in reducing symptoms, schizophrenia is not just a medical issue; it’s a bio-psycho-social condition, says Dr. Khanna.
“Biologically, there’s a chemical imbalance in the brain. Psychologically, factors like childhood trauma or poor coping mechanisms contribute. And socially, how families and communities treat the person plays a huge role.” This means recovery needs more than pills. It needs psychotherapy, social support, family involvement, and community acceptance.
“You can’t just give someone medicine and leave them to figure out the rest. Healing is a holistic process.”
 Dr Sharma points out that in genetically vulnerable individuals, trauma can serve as a trigger
Dr Sharma points out that in genetically vulnerable individuals, trauma can serve as a trigger
Dr. Sharma further explains the link between trauma and schizophrenia: “While schizophrenia is a neurodevelopmental disorder with biological roots, trauma acts as a major environmental risk factor that can influence both the onset and severity of symptoms.”
“Early trauma disrupts brain development. Experiences like emotional neglect, abuse, or parental loss can alter brain pathways involved in stress and emotion, all of which are implicated in schizophrenia,” she says.
She also points out that in genetically vulnerable individuals, trauma can serve as a trigger. “Chronic trauma may affect self-concept and social trust, leading to isolation and emotional dysregulation — all of which can worsen or mimic psychotic symptoms.”
Recognising and addressing trauma, she stresses, is vital for holistic, person-centred care.
The recovery often involves:
• Medication (primarily antipsychotics),
• Psychotherapy (especially CBT for psychosis),
• Social skills training,
• Family support and psychoeducation, and
• Rehabilitation services (vocational and community support).
Myth 5: “They’ll never get better”
This belief can be especially harmful, and simply isn’t true. While schizophrenia is a chronic condition, many people improve significantly over time with the right combination of care and support. Some achieve what doctors call “functional recovery”, where they can manage symptoms and live full, independent lives.
“I wish more people understood that schizophrenia isn’t the end,” says Dr. Khanna. “Yes, it’s a long journey. But it’s a journey people can walk and thrive through, if they’re supported.”
Dr. Sharma echoes this: “When society understands that schizophrenia is not about demons or split minds, but a treatable condition, we can build systems that offer real hope.”
Changing the way we see schizophrenia
The danger of misinformation isn’t just confusion — it’s neglect, discrimination, and delayed care. Across India, an estimated 3 in every 1,000 people live with schizophrenia, according to the National Mental Health Survey (2015–16). That’s over 4 million people, many of whom never receive a formal diagnosis or access to consistent treatment.
Despite the availability of treatment options, nearly 75% of people with severe mental disorders in India, including schizophrenia, do not receive any mental health care, as highlighted by the World Health Organisation (WHO). Often, it’s not the illness itself but the fear, silence, and stigma surrounding it that keep people from reaching out for help.
 While schizophrenia is a chronic condition, many people improve significantly over time with the right combination of care and support.
While schizophrenia is a chronic condition, many people improve significantly over time with the right combination of care and support.
Behind every missed diagnosis is someone trying to cope — often alone — while the world looks away.
But change starts with awareness.
“We need to stop seeing people with schizophrenia as their diagnosis,” says Dr. Khanna. “They’re individuals — with strengths, stories, families, and dreams. If we shift our approach, we can change their lives.”
By breaking the myths, opening up conversations, and replacing judgement with empathy, we can help more people find not just treatment, but dignity, purpose, and belonging.
The journey toward understanding schizophrenia doesn’t end with reading an article. It begins there.
Learn the difference between fact and fiction. Listen to lived experiences. Talk to someone. Support organisations working in the mental health space. Small steps like respectful language can help chip away at decades of stigma.
Because when we choose to understand, we give people more than treatment — we offer them dignity, connection, and hope.
Edited by Leila Badyari
News